Artificial Intelligence Is Revolutionizing Patient Care
Artificial intelligence (AI) is making remarkable strides in revolutionizing patient care. With its transformative capabilities, AI is reshaping healthcare by enhancing the accuracy of diagnostics, optimizing treatment planning, and predicting patient outcomes.
The global market for healthcare AI was valued at $15.4 billion in 2022, and it is projected to experience significant growth with a compound annual growth rate (CAGR) of 37.5% from 2023 to 2030.
In this article, we will explore how artificial intelligence is revolutionizing patient care, ultimately leading to improved healthcare outcomes and patient engagement.
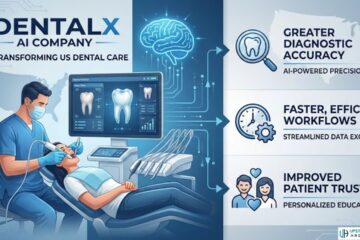
1. AI in Diagnosis
Research shows that between 40,000 and 80,000 deaths in American hospitals may be attributed to misdiagnosis. However, this number can decrease with the use of AI in diagnosis.
How Machine Learning Is Improving Accuracy and Speed of Diagnosis
Doctors can now rapidly and accurately diagnose diseases with the help of machine learning. Machine learning (ML) uses advanced algorithms to analyze patients’ data and identify patterns and anomalies that might be difficult for human doctors to detect. It then makes predictions based on the data.
By leveraging the power of large datasets and sophisticated algorithms, healthcare providers can make more informed decisions and provide better care promptly. This is especially necessary with rare or difficult-to-diagnose diseases such as cancer. For example, ML can analyze images to detect cancer early.
ML can help eliminate human error, which may come due to fatigue due to work overload or misinterpretation of patient data. AI’s ability to diagnose a disease early enables health providers to prioritize high-risk cases, which can reduce the mortality rate.
With an accurate diagnosis, doctors can then go through the proper channels of treatment to ensure that the patient is getting the help they need to support them through this. Just because AI plays a big part, does not mean doctors are not on the ball themselves. They will need to catalogue a code for a specific ailment (you can learn how to code for chronic neck pain through websites such as The Intake to better understand this process), as well as keep constant updates so they know if there is any progress or if another diagnosis is needed for the next stage.
Applications of AI in Medical Imaging and Pathology
Medical imaging is one of the doctors’ most valuable data to determine a patient’s condition. Data from computerized tomography (CT) scans, magnetic resonance imaging (MRI), mammography, and ultrasound, among others, can sometimes be complex.
Complex data may take time to be interpreted and even risk misinterpretation. However, the use of AI by radiologists and pathologists is improving turnaround time since it can quickly recognize and identify image patterns. It also improves their accuracy and efficiency, minimizing patient wait times and costs. For patients seeking reliable diagnostic services, options like medical imaging in West Orange, NJ, or a local alternative provide access to cutting-edge technology and expertise, ensuring timely and accurate results.
An excellent example of how AI is used in radiology is its application in automated tumor and organ segmentation during radiation.

Benefits of AI in the Early Detection and Prevention of Diseases
AI helps in the early detection and prevention of diseases and makes it easier for healthcare professionals to develop treatment plans easily. It also helps patients to recuperate on time and prevent complications that may arise due to late diagnosis.
Wearable technology, such as smartwatches, plays a crucial role in the early detection of illnesses or health conditions that doctors may take time to detect. This is by monitoring health vitals such as temperature, heart rate, skin temperature, blood pressure, or blood sugar levels.
Among the diseases AI can diagnose are:
- Cancer
- Diabetes
- Alzheimer
- Stroke
- Chronic
- Heart disease
- Skin disease
- Arrhythmia disease
- Cerebrovascular
- Hypertension
- Skin
- Liver disease, and more.
AI significantly impacts predictive medicine, which uses patient data to predict future health risks and outcomes through patterns and trends. This allows for prevention, early diagnosis, and the development of more effective treatments. For example, AI can predict a patient’s risk for cardiovascular disease, epilepsy, or cancer better than traditional methods.
2. AI in Treatment
Research shows that patients respond differently to medicines hence the need to personalize their treatment plans. This makes it crucial for doctors to personalize treatments for each patient, even if they have the same diagnosis.
The Role of AI in Personalized Treatment Plans
Personalized treatment requires a deep understanding of the patient’s condition, which means analyzing large amounts of data, which can be challenging for healthcare providers. Artificial intelligence can help develop personalized treatment plans by analyzing a patient’s medical history, test results, family history, and other patient characteristics. It then uses the information to predict a treatment plan, including the dosage required.
AI can also monitor a patient’s progress and suggest adjustments to the treatment plan depending on the patient’s responsiveness.
Artificial intelligence can also be used in precision medicine, which uses a patient’s genetic makeup to diagnose, prevent, or treat a disease. Precision medicine has been effective in some cancers, rare genetic disorders, and the management of chronic diseases such as cardiovascular diseases and diabetes.
AI in Drug Development and Therapies
Machine learning algorithms can identify new drug targets, optimize their efficacy, and analyze potential side effects. Drug discovery and development is a costly and time-consuming process.
According to Harvard Medical School, developing a new drug can take 11 to 16 years and $1 billion to $2 billion. However, AI can help cut these costs and time by quickly analyzing massive amounts of biochemical data. It helps in preclinical research, wet lab experiments, and clinical trials.
ML also supports the design of new therapeutic modalities, especially for rarer and more complex diseases. It can give accurate predictions on protein and gene therapies, among others.
Reduction of Medical Errors and Improving Treatment Outcomes
There have been numerous instances where doctors have prescribed the incorrect drug, worsening patient conditions or even causing death. So, besides machine learning reducing errors associated with the traditional trial-and-error approach during development, it also decreases medication-related errors.
Accurately developing and predicting drugs and therapies helps healthcare providers give effective treatment. As a result, there will be more efficiency in patient care by improving treatment outcomes and overall patient survival.
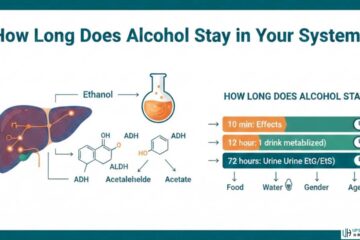
3. AI in Patient Monitoring
AI has become a powerful tool in patient monitoring, enabling healthcare providers to monitor their patients continuously, no matter their location.
Applications of AI in Remote Patient Monitoring
Remote patient monitoring (RPM) or telemonitoring has been made possible by AI-powered devices. RPM allows healthcare providers to monitor patients even if they are not in the same room as the patient. For example, they can monitor the patient’s healing progress outside traditional clinical settings.
Remote monitoring can be done through wearable devices, sensors, or mobile apps for telehealth platforms. RPM makes the management of chronic or acute illnesses easier since it offers continuous and real-time monitoring of patient’s vital signals or psychological parameters.
Remote monitoring also aids in detecting patterns or conditions that a routine medical examination cannot pick. It then alerts health providers if it detects issues, enabling them to take appropriate action before things worsen.
Benefits of AI in Predicting and Preventing Adverse Events
Remote monitoring enables patients to better understand their condition since they will engage more with their health providers. There will also be adherence to treatment plans and medical routines due to improved communication between patient and provider. AI can also help set reminders and recommend lifestyle changes to ensure patient adherence.
Chronic illnesses account for 80% of hospital admissions, and remote patient monitoring can help reduce this rate. According to the American Heart Association (AHA), RPM can effectively monitor cardiovascular risk factors and conditions, including hypertension, heart failure, and atrial fibrillation.
Remote patient monitoring is also effective at diabetes monitoring by spotting patterns and behaviors that may lead to an increase or decrease in blood sugar levels. Devices such as AI-powered insulin pumps can help monitor a patient’s blood sugar levels and adjust insulin doses accordingly.
Virtual and Voice Assistants in Remote Monitoring
With the ever-growing rate of the elderly population, virtual and voice assistants can be helpful and play a significant role in remote patient monitoring. These assistants can provide patients with easy access to medical information and education. They also reduce loneliness in elderly patients.
The Potential of AI in Reducing Healthcare Costs
Using AI in patient care increases patient outcomes since they will have an accurate diagnosis and receive personalized treatment plans. Besides reducing hospital admissions, predicting and preventing adverse health events minimizes costs for treatment.
Remote monitoring increases patient engagement and adherence, which can result in improved contentment and comfort, eventually leading to high patient outcomes. As a result, positive patient outcomes minimize the need for hospital readmissions and emergency department visits, reducing patient and healthcare costs.

Remote patient monitoring can also help patients who prefer outpatient rehabilitation (which is cheaper) when recovering from substance abuse. This can be through a device such as a smart band that provides clinical insights and analytics to providers.
4. Ethical Considerations
As healthcare continues to use AI in different healthcare fields, it’s important to consider the ethical implications that may come with it. After all, AI is only as good as the data it’s given, and if that data is biased, AI can perpetuate those biases. It may also breach a patient’s privacy and confidentiality.
Addressing Ethical Concerns in Using AI in Patient Care
According to the World Health Organization (WHO), AI must work for the public good by ensuring ethics and human rights are met in its use. The growing use of AI raises ethical concerns such as consent, safety and transparency, privacy, and fairness, which must all be addressed.
The role of eliminating these issues mainly lies with developers and healthcare providers. AI systems should be highly trained on diverse datasets. Developers should also ensure their algorithms are transparent and accountable.
Ensuring Patient Privacy and Confidentiality
Vendors’ due diligence is crucial to understanding the system and ensuring patient privacy and confidentiality. There should be a confirmation of how patient data is recorded and accessed. Controls should be in place to access patient data, and patients must have the right to information before medical procedures or treatment begins.
Since AI runs on automated instructions, developers should ensure the full implementation of policies, procedures, and security measures. Healthcare providers can also review recommendations and monitor AI to prevent ethical issues.
As policymakers worldwide continue to develop more guidelines, healthcare providers and developers are required to abide by those that are currently in place.
Balancing the Benefits of AI With Human Interaction
As AI use continues to evolve in the healthcare industry, it’s important to remember human interaction and empathy are still crucial. Empathy, trust, and compassion are essential for creating a positive doctor-patient relationship. Patients who feel understood and cared for are more likely to continue their treatment plans and follow doctors’ orders, resulting in better health outcomes.
So, AI should not be a replacement for human interaction. Instead, it should be a way to supplement and enhance healthcare professionals’ care. Combining the best of both worlds makes the healthcare system more efficient and effective.
Conclusion
AI is changing the landscape of patient care for the better. It can help doctors diagnose patients faster and more accurately and create personalized patient care plans. AI can also develop new treatments and drugs, reducing costs and speeding up the process. Overall, AI is improving patient safety and reducing patient and healthcare costs.
AI adoption in healthcare has been slow; some healthcare professionals are worried about being replaced by AI. Others are bothered about the ethical implications of using AI in healthcare. However, the highlighted benefits indicate that AI can streamline workflows and reduce health providers’ tasks, thus, improving patient care.
For AI to be successful in healthcare, ethical concerns should be addressed. This should be from developers to end users to organizations responsible for enacting regulations. Maintaining a human-centered approach to patient care can be crucial in addressing ethical concerns.
See Also: 9 Best AI Writing Tools in 2023: Improved Content Creation